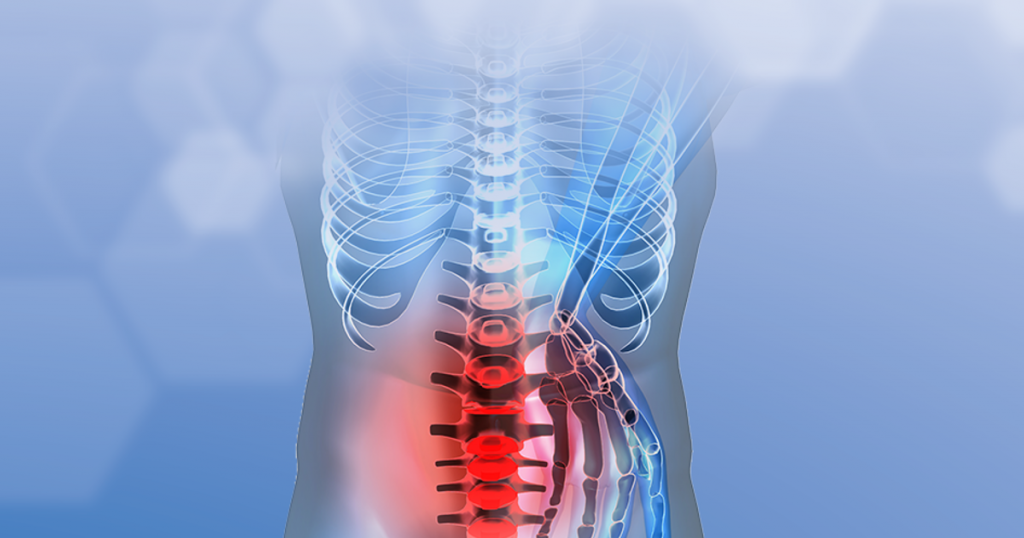
When you have been suffering from back pain, surgery may be a welcome relief. But what does it mean when surgery fails, and you have back pain that won’t go away?
You may be experiencing failed back surgery syndrome (also known as FBSS or failed back syndrome). The name is a little misleading—it’s not actually a syndrome. It’s a general term describing patients who have not had relief from spine surgery.
If you have failed back surgery syndrome, there is still hope for treating your lingering back pain.
Pain Right After Surgery
First of all, it’s important to note that some back pain after surgery is normal.
According to Veena Graff, MD, MS, Anesthesiologist and Pain Medicine Physician at Penn Medicine, most people experience some pain right after surgery, especially during the first 24 to 72 hours. While every patient is different, many patients notice the pain beginning to subside after this time—but that doesn’t mean instant relief.
Full recovery, however, can generally take about 4 to 6 weeks, and you might continue to have mild to moderate pain during this period. But don’t be discouraged—it’s a normal part of recovery,” Dr. Graff says.
If significantly more time than that has passed—and the pain seems to be more like your original pain rather than post-op pain—it may be time to start considering your options.
Taking the First Step
Don’t assume that all hope is lost, and do not start self-medicating. The very first thing you should do is confirm that it’s not lingering post-op pain.
If the pain lingers beyond the general 4- to 6-week recovery period, it’s not necessarily bad news—recovery is a little different for everyone,” Dr. Graff says. “But if the pain persists, it’s important to follow up with your surgeon to be screened in person to re-evaluate why the pain is continuing.
If you’re receiving treatment at Penn, your surgeon may recommend additional imaging, or a consultation with the Penn Medicine Pain Clinic.
If your surgeon has confirmed that the pain is not just lingering post-op pain, try not to get discouraged. Surgery may not have fully corrected your pain, but that doesn’t mean that you will never be able to control it.
Pain Management: Medication
Right after surgery, your surgeon will prescribe medication to relieve pain. Dr. Graff says. It’s possible that you will continue on some of your medications if the pain persists.
There are many different categories of pain medications,” explains Dr. Graff. “We may prescribe anti-inflammatory drugs, nerve pain-reducing medications, drugs that work on various types of pain receptors, and/or medications that release neurochemicals that help reduce pain.
Antidepressants and anti-seizure medications may have properties that relieve pain, but they won’t work as well if taken on an “as-needed basis.” They need to be taken regularly, whether or not you’re in pain.
However, there is one medication you will not be prescribed long-term. Opioids are powerful medications that are indicated for severe pain, and they may be prescribed for a temporary period after surgery. But prolonged opioid use can lead to abuse and addiction. So patients normally don’t receive long-term opioid prescriptions for back pain.
Pain Medication: Medication via Epidural
You have probably heard of epidurals as a source of relief for women going through labor. But they aren’t just used in childbirth. Epidurals are sometimes used as a treatment for chronic back pain that is not corrected by surgery
If you receive an epidural, you will get an injection of medication into the epidural space—the space around the spinal cord. The medication can reduce swelling and pain around damaged nerves, and in and around the spinal nerve roots.
Not all patients react the same to this procedure. For some, an epidural will provide long-term relief. For patients who experience short-term relief, they may need another round of injections later on.
Pain Management: Physical Therapy
A major part of the healing process is getting back to physical activity,” Dr. Graff says. After surgery, a physical therapist will prescribe certain exercises to help you regain strength and mobility.
If you have gotten back to your normal activity, but you’re still in pain, one option is to continue with physical therapy.

There are two types of physical therapy: Active and passive.
Active physical therapy is exercise-based. This type of therapy is usually comprised of a few different components. Your physical therapist will work with you on stretching, strengthening, and low-impact aerobic conditioning (e.g., walking, swimming).
Passive physical therapy is therapy done to a patient, not by a patient. It can involve ice, heating, steroids applied to the skin (iontophoresis), electrical nerve stimulation, and ultrasound.
While it’s important to follow your physical therapist’s recommendations, and not try therapy by yourself, there is one form of passive physical therapy that you can probably try on your own—heat and ice.
Both heat and ice can be very beneficial for pain management,” Dr. Graff says. “Heat is typically used to relax muscles or joints that feel stiff, and ice is usually used when there is an acute pain flare-up and inflammation. Ice has a numbing effect, so it is often recommended shortly after having a surgical procedure to reduce the acute pain and inflammation.
As healing takes place over time, you can use heat or ice, depending on your personal preference.

